RESEARCH REPORT
|
|
Access the article online: https://kjponline.com/index.php/kjp/article/view/530 doi:10.30834/KJP.38.1.2025.530 Received on:23/05/2024 Accepted on: 20/07/2025 Web Published:23/07/2025 |
PSYCHOSOCIAL PROBLEMS AMONG HEALTHCARE WORKERS IN A TERTIARY CARE CENTRE DURING THE COVID-19 PANDEMIC: A QUALITATIVE STUDY
Indu PV1*, Harish M Tharayil2, Chitra Dilip3, Anithakumari Ayirolimeethal4, Harsha Vadakkechalil5, Anu Padmanabhan6, Afeefa Moidu7, Rajula KP8, Aysha Zabin Madathil9, Varsha Vidyadharan10
- Professor, Department of Psychiatry, Government Medical College, Thiruvanathapuram, 2. Professor, Department of Psychiatry, KMCT Medical College, Kozhikode 3. Special Registrar, Essex Partnership University NHS Foundation Trust, UK. 4. Professor, Department of Psychiatry, Government Medical College, Kannur, 5. Consultant Psychiatrist, KR Clinic, Chungam, Feroke, Kozhikode, Kerala, India, 6. Assistant Professor, Department of Psychiatry, KMCT Medical College, Kozhikode, 7. Consultant Psychiatrist, Fathima Hospital, Kozhikode, 8. Assistant Professor, Department of Psychiatry, PK Das Institute of Medical Sciences, Vaniamkulam, Palakkad, Kerala, India, 9. Specialty Doctor, Tees Esk and Wear Valleys, NHS Foundation Trust, UK, 10. Assistant Professor, Department of Psychiatry, Government Medical College, Kozhikode
*Corresponding Author: Professor, Department of Psychiatry, Government Medical College, Thiruvanathapuram, Kerala.
Email: indupv2013@gmail.com
INTRODUCTION
The coronavirus (COVID-19) pandemic of 2019 was an unparalleled international public health emergency that has left an indelible impact on mankind, not only through its biological effects but also through the socioeconomic and psychosocial repercussions.1 Healthcare workers (HCWs) are a highly vulnerable population for psychological consequences related to pandemics or epidemics. High rates of depression, anxiety, and emotional distress have been reported in HCWs during these pandemics due to the tremendous stress that they experienced, due to the risk of infection, workload, perceived stigma, quarantine, etc.2
In a meta-analysis to assess the psychological impact of the COVID-19 pandemic on HCWs, the pooled prevalence of anxiety was found to be 37%, and that of depression was 36%.3 In another meta-analysis, a qualitative synthesis of the information from nine studies revealed the apprehensions of HCWs about acquiring the infection, transmitting it to family members, and the quarantine.4 A mixed-methods study in Malawi on frontline HCWs, in the qualitative phase, found emotional distress, impact on personal life and work, stigma, and discrimination as the major issues.5 A mixed-methods systematic review that assessed the mental health outcomes of HCWs in India during the pandemic identified the fear of getting infected, spreading it to their family, physical exhaustion, social stigma, and concerns regarding the personal protective equipment (PPE) as the major themes.6 In an updated meta-analysis assessing the mental health repercussions of the pandemic among HCWs in India, more than one-third of them had mild to severe depression and anxiety.7 Other cross-sectional web-based/online studies done in India during the pandemic found high rates of anxiety, depression, or both among HCWs.8,9 Most of these studies were quantitative studies, conducted online.
In a mixed-methods study of HCWs delivering care in a slum in India, an ethnographic study found that fear of death, guilt of infecting loved ones, stigma from the community, and exhaustion were the major themes leading to stress in this population.10 In a qualitative study done in Dhaka, 15 IDIs were conducted with healthcare professionals over the telephone. Heavy workload, psychological distress, poor quality of PPE, social stigma, and improper management strategies were some of the themes identified.11 Another qualitative study conducted among HCWs reported work-related and family-related challenges, psychological distress, and use of various coping strategies in this population.12 A study done on physicians all over India using virtual IDIs reported fear of infection, uncertainty, stigma, guilt, and social isolation as their main challenges. Their unmet needs and resilience framework were also studied.13 Many of these studies were conducted online or over the telephone. None of these studies reported the perspective of the residents who were involved in providing healthcare during the pandemic. Hence, a qualitative study was done in a tertiary care teaching hospital to explore the psychosocial problems faced by the HCWs, including residents, during the COVID-19 pandemic.
MATERIALS AND METHODS
This qualitative study was undertaken as a part of a mixed-methods study to assess the psychological problems in HCWs during the COVID-19 pandemic in a tertiary care centre. The objective of this qualitative study was to have an in-depth understanding of psychosocial problems experienced by the HCWs engaged in delivering care to COVID-19 suspected or positive cases in the Government Medical College, Kozhikode, Kerala; and also to explore their preoccupations, apprehensions, and felt needs. The study was undertaken over nine months starting from March 2021. Eleven In-depth Interviews (IDIs) and four Focus Group Discussions (FGDs) were conducted, including various stakeholders, after obtaining the participants' written informed consent. FGD guides and IDI schedules were prepared separately by IPV and validated by expert review by HMT, AA, VV, and an expert in qualitative research.
Participants: The stakeholders for IDIs included the Principal, Vice-principal, Superintendent of the hospital (who was also the Chief Nodal Officer), the Assistant Nodal Officer, the Nursing Superintendent of the hospital, the heads of the departments of Respiratory Medicine and Forensic Medicine, a Medical Officer from the department of Internal Medicine, a Junior Resident from the department of Respiratory Medicine, a staff nurse, and an attender. FGDs were conducted separately for homogeneous groups of residents, staff nurses, nursing assistants, and grade II attenders. There were six participants in each FGD, selected purposively to ensure representation from various departments. (Table 1) The number of IDIs and FGDs was decided based on attaining redundancy of information.
Table 1. Sociodemographic details of the participants in Focus Group Discussions (FGDs)
|
FGDs |
Range of age |
Gender distribution |
Educational status |
|
Residents |
25-36 years |
2 males, 4 females |
MD – 1 (Senior resident) MD/MS students – 5 |
|
Staff nurses |
29-41 years |
2 males, 4 females |
BSc Nursing – 4 General Nursing – 2 |
|
Nursing assistants |
46-57 years |
3 males, 3 females |
SSLC – 6 |
|
Grade II attenders |
43-56 years |
5 males, 1 female |
SSLC – 5, Degree – 1 |
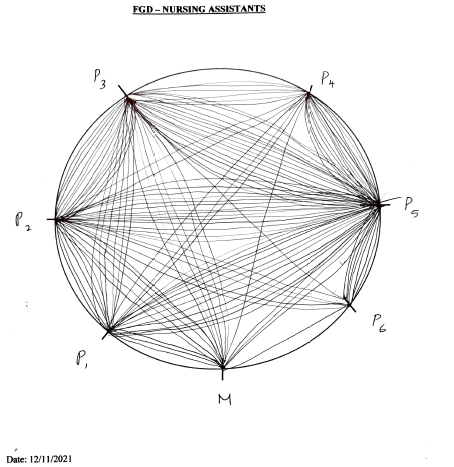
Data collection: The IDIs were conducted by IPV and HMT. The moderator for the FGDs was IPV, who was trained in qualitative research methodology. IPV contacted the participants in advance, confirmed the venue and time of the interview or discussion, and ensured their participation. One junior resident and one grade II attender could not attend the FGD due to personal reasons. The IDIs and FGDs were conducted face-to-face at the tertiary care center and recorded using voice recorders, after obtaining informed consent from the participants. Each IDI and FGD lasted 45-90 minutes. A rapporteur documented the interviews and discussions manually; another observer drew sociograms for all the FGDs. (Figure 1)
Figure 1. Sociogram of the Focus Group Discussion of Nursing Assistants
Data analysis: The IDIs and FGDs were transcribed into the local language, translated into English, and thematic analysis was done manually. After familiarizing themselves with the data, IPV, HMT, AA, and VV independently conducted free-listing of responses, domain identification, and coding. Furthermore, the same team of investigators undertook discussions, identified, defined, and named categories and themes, and developed a conceptual model through thematic analysis using an inductive approach. Triangulation of methods, data, and researchers was ensured.
RESULTS
The main stakeholders for the IDIs were the administrators, faculty members, a resident, a staff nurse, and an attender. The FGDs were conducted for homogeneous groups of residents, nurses, nursing assistants, and grade II attenders, with six participants each. Overall, there were 12 males and 12 females; their ages ranged from 25 to 56 years, and they were educated up to the SSLC level and above, including professionals such as nurses and doctors (residents). The main themes identified included physical, emotional, behavioral, interpersonal, interdepartmental, occupational, social, and academic problems, as well as worries and apprehensions, and deficiencies in various fields.
Physical problems
Almost all the participants reported physical problems, mostly related to wearing the PPE. The majority of participants reported experiencing excessive heat and sweating, severe dehydration, fatigue, and exhaustion while wearing the PPE. Headache, hypotension, syncope, dizziness, dyspnoea, menstrual irregularities, urinary tract infections, allergy, pressure sore on the nose, etc., were some of the main problems. Problems in functioning due to the goggles getting fogged, difficulty in climbing stairs, difficulty during menstrual periods, and inability to take food or water were reported to be associated with PPE usage. Weight gain due to binge eating, aches and pains, nausea, vomiting, and palpitations were some of the issues unrelated to PPE. The administrators expressed difficulties related to attending 400-450 calls per day and attending calls in the middle of the night, which used to affect their sleep.
“When we wear the PPE, there is difficulty in taking breath. So also, other problems like sweating, thirst, and fatigue…. Some skin problems were related to wearing gloves.”
— 43-year-old, male, Grade II attender, FGD
“There is difficulty in working while wearing the PPE. … Reports feeling tired soon. We are not able to take food or water; for six hours, we have duties like that.”
- 29-year-old, female Nursing Officer, FGD
Emotional problems
Almost all the participants reported emotional problems like anxiety, fear, depression, anger outbursts, mood swings, apathy, and guilt feelings. Most of the problems were related to their work or family. Initially, they had fear or anxiety of getting infected; later, of infecting their family members. The residents reported anxiety and palpitation when the monitors beep in the intensive care units (ICUs); the attenders were scared of the possibility of running out of oxygen while shifting patients on trolleys. Watching air hunger in the patients and watching them die, especially the young ones without much health issues, led to frustration, guilt, anxiety, and depression in the residents and medical officers. They had guilt and anxiety, not only about not doing enough for the patients, but also about not doing their duty towards their family. Almost all the participants mentioned that they had anger outbursts, mostly due to the excessive workload and the discomfort of wearing PPE, which they displaced onto their colleagues, not patients. The administrators had experienced a lot of pressure from higher authorities, which led to excessive mental stress and fear of taking on their duties.
“Those below 50 years – we expect them to survive, somehow. Seeing them die; the second wave was terribly different that way. Mortality is high in younger age, in those without comorbidities. … We become desperate that we can’t do anything.”
— Medical Officer, General Medicine, and Former Assistant Nodal Officer, IDI
Worries and apprehensions
All the participants reported worries and apprehensions regarding getting infected while caring for the patients, being exposed to their secretions, when the PPE gets torn, or when they experience fatigue. They had greater worries of infecting their family, especially children and the elderly. In the initial phase, lack of awareness or knowledge regarding the disease and its management was the greatest worry. They were plagued by feelings of guilt for not being able to give adequate care to patients and not being able to fulfill their responsibility towards their families. They also felt that they were not wanted at home and were a burden to their families. They were losing their friendships; their social life was getting compromised. In the second wave of COVID-19, which was more virulent and associated with a larger number of deaths, many of them reported feelings of helplessness and hopelessness. The residents reported a state of learned helplessness – that there is no benefit in doing anything for the patients. They were apprehensive about how long the pandemic would last. Their academic activities and training were getting affected. They were unable to concentrate on or remember things. All the participants reported being overwhelmed by the workload. The administrators were concerned about managing the deficiencies in all fields – manpower, oxygen supply, PPEs, etc.
“When I sedate and paralyse a patient for intubation, when I look at the patient, I have often thought that mine would be the last face that he is gonna see. Can say that it was severely traumatic. … Had to intubate with that feeling of helplessness.”
— Male Senior Resident from General Medicine, FGD
“There is a feeling that we can’t do anything productive. When we do something for patients, what is the purpose of doing it? If they become sick, there is no benefit in our doing anything particularly.”
—Female Junior Resident from Respiratory Medicine, IDI
Behavioral problems
Various behavioral problems were reported by all the stakeholders. Avoidance behavior, like taking leaves, shirking responsibilities, and not taking care of the needs of the family, was reported mostly by the staff nurses, nursing assistants, and grade II attenders. The nursing staff reported insubordination among their subordinates. More complaining behavior was observed – about having more duties and even about the quality of food provided. Each group was found blaming the others for shortcomings in their work. Inappropriate behaviors like anger outbursts at superiors were reported, but were rare. Risk-taking behaviors like removing the mask to drink water, binge eating, and eating junk food were described by the junior residents. None of the stakeholders reported worsening of alcohol use, but some reported an increase in smoking to relieve tension. All the stakeholders reported a lack of cooperation from higher authorities.
“When we go for the second duty, the porridge that had to be given at noon would be left there, for the next person who comes for duty to grind it in the mixie and give. So, one’s job is kept aside for another person.”
— 49-year-old, male Nursing Assistant, FGD
Interpersonal problems
All the participants reported interpersonal problems with their family, colleagues, superiors/subordinates, and even the patients and/or their bystanders or relatives. Staying away from the family for months, not communicating with them, neglecting family responsibilities, and avoiding household chores were problematic for most stakeholders. While doctors reported being irritable to their family members, not other staff members, other HCWs reported being irritable to colleagues, not patients. Most stakeholders felt that their superiors did not understand and would not inquire about their well-being. Staff nurses, nursing assistants, and grade II attendants reported that their superiors blamed them for problems or mistakes, and this would cascade downwards. They opined that the language of the superiors could be more tender. The junior residents felt that there was a lack of concern from faculty members and department heads; they were not understanding their suffering or considering their workload. They just wanted the job to be done, for things to go on; they were not interested in how it was done. The nursing assistants and grade II attenders had a good relationship with the patients and their relatives, and the latter appreciated the help that they received from the staff. The residents were more defensive in answering the relatives' queries, considering the unpredictable course of the illness. The middle-level administrators felt that there was a lack of cooperation not only from higher authorities, but also from their subordinates in implementing the decisions taken. They thought that the adverse comments of the superior authorities added to their stress.
“I did not have any interaction with my child due to COVID. And my child has cerebral palsy, for which behavioral training and all were needed …. It got delayed.”
— Female Junior Resident from Psychiatry, FGD
Interdepartmental problems
The doctors and the administrators reported these. It was observed that interdepartmental relationships deteriorated due to the COVID-19 pandemic. As the department of Internal Medicine could not cope with the workload, other clinical and non-clinical departments were also involved in providing care. Those from other clinical and non-clinical departments found it difficult to cope with COVID-related problems due to their lack of competency in handling such issues. Such departments felt exploited, leading to even heated arguments between department heads and faculty members regarding the duties assigned to them. Some accused the higher authorities of being partial to some departments. The middle-level administrators felt that adverse comments from those who were seen as friends earlier, even in WhatsApp groups, were a mental stress. There were adverse experiences, including misbehaviour and verbal abuse, from colleagues in other departments. Many reported a loss of friendly relationships with other departments.
“If we ask those who don’t know things to work in this scenario, nobody would like to do so. E.g., if we ask Dermatology people to take Corona duty, they don’t know how to manage …. The strain is on Medicine people, and there is clash. … Inter-departmental relationships have become bad due to Corona.”
— Vice Principal, IDI
Social problems
These were reported more frequently by nurses, nursing assistants, and grade II attendants. The local people avoided speaking to these HCWs, even to their children. Some people would not use the common tap used by them, and would move aside when they went to shops. They would not have been able to get houses for rent or had to change their rented houses. Many of them experienced disregard from friends and neighbors due to the social stigma associated with COVID-19. They had to keep away, avoid going out of their homes, remain in their rooms, instruct their children not to go out, and even refrain from informing others that they were taking on COVID duty. They felt socially isolated and ostracized. Doctors did not report such problems. Other social problems reported included financial difficulties observed in every household, with everything at a standstill. Some stakeholders observed that many of the staff members recruited under the National Health Mission (NHM) were highly educated, including professionals, postgraduates, and postdoctoral candidates. As they had no other jobs or had lost their jobs, they were engaging in even the most menial work under the NHM.
“If we go to take a house, they ask where you are having duty. If we say 'Medical College' and 'Corona duty,' they don’t give us accommodation. … When they understand that we are staff with Corona duty, I had to change my house three times because of this.”
— 29-year-old, female Nursing Officer, FGD
Deficiencies
All the stakeholders reported deficiencies in manpower, training, infrastructure, and materials. The junior residents reported an acute shortage of postgraduate trainees, with one resident caring for up to 50 patients in some departments. In such circumstances, it was not possible to give adequate or individualized care to patients. The deficiency of HCWs was exacerbated when the staff were relocated to other institutions and when one batch of residents left after completing their course. The staff members recruited via NHM were not adequately trained and did not receive adequate supervision. The management of ICUs by inadequately trained staff would lead to wastage of materials, damage to ventilators, and even the death of patients.
There were deficiencies in the infrastructure, an inadequate number of beds in the ICU, a lack of isolation wards, a lack of space, an inadequate freezer facility to keep COVID-positive and -negative bodies separately, insufficient cooling in the mortuary leading to decomposition of bodies, etc. Deficiencies of materials like gloves, masks, sanitizers, PPEs, medicines, materials for intubation, and even water were reported by all the stakeholders. Maintenance work was also inadequate – there was a delay in rectifying even the malfunctioning ventilators.
“It is difficult to manage with the available manpower. There are six-hourly duties, ,,, it is additional to their routine work for MOs, PGs, or staff nurses. We cannot manage with the available PGs or permanent staff.”
— Chief Nodal Officer and Former Superintendent, IDI
Deficiencies in academics
The residents and some of the medical officers reported that the postgraduate academic activities were affected. Their training was paused; there were no bedside clinics or case discussions. Those in surgical specialties were apprehensive that they were not learning to do procedures or acquire new skills. Due to the workload and associated physical problems, the residents were tired, sleepy, and unable to pursue their academics. There was a lack of motivation to learn. They felt that they were far removed from the subjects they wanted to pursue, and some even considered discontinuing their course. They were apprehensive that they had not begun their thesis work. They felt that they had no academic benefit and were being used solely for documentation purposes. The undergraduate teaching and training of house surgeons were also affected badly. The extension of the internship period affected their hopes of pursuing their academics further. This added to their frustration.
“We don’t know anything about our subject. So, the main apprehension now is “What next?” We won’t be good doctors when we go out.”
— Female Junior Resident, Obstetrics & Gynecology, FGD
Problems in occupational functioning
All stakeholders reported being overwhelmed by the workload. A shortage of manpower, increased patient load, and hectic duty schedules affected the functioning of all stakeholders. The residents had 24-hour duties once or twice per week. The wards and ICUs were full, and proper care could not be given to the patients. A larger number of deaths during the second wave affected the morale of the HCWs. The timings of night duty, until 1:30 am, and after that, were causing issues with the safety of HCWs, especially women, when traveling alone before and after duty hours. The administrators reported that they had problems with attending to hundreds of calls every day. They had to answer many questions, give suggestions, and implement the decisions taken, and they were mostly held responsible for the deaths. Moreover, they felt that the superior authorities were not cooperative.
“There are people who say they can’t cope. They say that there are almost 20-29 patients, and only two staff. Should we administer medicine, go on rounds, or provide care to the patients? They say that they are unable to give patient care.”
— 38-year-old, female Staff Nurse, IDI
Coping strategies
Most of the administrators reported that they were able to face the pandemic despite the deficiencies. As and when problems arose, they could find solutions; when patients in isolation made demands, such as for food, hot water, or chargers for mobile phones, etc., were arranged through sponsorship. They could arrange counselling for HCWs with psychological problems. Manpower shortage could be addressed by recruiting personnel via NHM, and by appointing caregivers or permitting bystanders to be with the patients. Classes for students could be arranged online and offline. Other stakeholders reported that repeatedly taking on duties had brought down their apprehensions. Increased awareness regarding the illness, taking vaccination, taking precautions against infecting family members, and avoiding going out or making visits were some of the strategies used by the HCWs to reduce their anxiety. Mostly problem-based coping strategies were employed.
“I haven’t gone home for months. I went home after two months. Even if I have it, I should not give it to my family. If family members get it, the local people will get it; the entire society will be affected. That should never happen. Had the thought that let us die if we get it, but others should not get it.”
— 47-year-old, male Grade II attender, FGD
Conceptual model
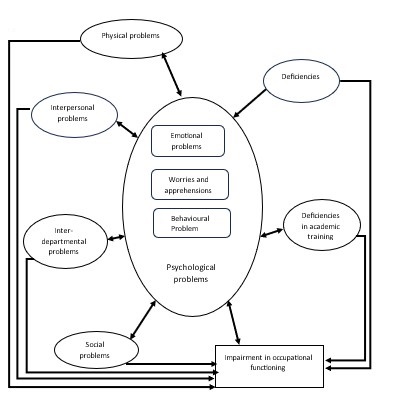
The physical, interpersonal, interdepartmental, and social problems experienced by HCWs during the COVID-19 pandemic were found to lead to psychological problems, including worries, apprehensions, emotional, and behavioral issues. The relationships mainly were bidirectional. Deficiencies faced by the HCWs, in various domains, added to their psychological problems. In the case of junior residents, the deficiencies in their academic training contributed to their psychological problems. All these factors led to impairment in the occupational functioning of HCWs directly, as well as indirectly through psychological problems. (See Table 2. and Fig.2).
![]()
Figure 2. Conceptual model of psychological problems in health care workers during the COVID-19 pandemic
DISCUSSION
This qualitative study was conducted to explore the psychosocial problems in HCWs during the COVID-19 pandemic. It was found that psychological problems, including emotional and behavioral ones, and various worries and apprehensions were prevalent among HCWs in this period. Different stakeholders, ranging from administrators to attendees, experienced stress due to physical, interpersonal, and interdepartmental issues. Social stigma and related issues were more prevalent among the staff nurses, nursing assistants, and attenders. Deficiencies in manpower, training, infrastructure, and materials plagued all the stakeholders. The junior residents were apprehensive regarding their lack of academic training. All the stakeholders were overwhelmed by the workload and excessive duties. Lack of understanding from higher authorities was reported by all the stakeholders.
Anxiety, fear, depression, anger outbursts, mood swings, apathy, and guilt feelings were reported by the stakeholders in this study. Various cross-sectional studies done worldwide and in India have reported high rates of anxiety, depression, and other psychological problems in healthcare workers during the pandemic.2,5,7,9 A multi-centric, cross-sectional, online survey conducted in India among doctors working in Corona wards reported moderate levels of depression, severe anxiety, and moderate levels of stress in about half of the participants.14 Another cross-sectional, web-based survey done among healthcare professionals across different states of India found a high prevalence of anxiety, depression, and stress. High levels of stress, workload, and lack of training were found to be the important reasons for psychological problems in this population.15 All these were quantitative studies conducted online. In the current qualitative study also, psychological problems, including emotional ones, were reported by all the stakeholders.
A comparative study of the mental health of healthcare professionals during the pandemic was conducted online in Germany, Austria, and Switzerland in 2020 and 2021. It was found that depression and anxiety persisted in the second pandemic year also.16 A longitudinal study done in Canada followed up the mental health of HCWs from COVID-19 till 2023. Over time, psychological distress and depersonalization increased, post-traumatic symptoms and personal accomplishment decreased, and emotional exhaustion did not show net change.17 In the present study also, psychological problems were reported by HCWs in 2021, the second year of the pandemic.
In a mixed-methods systematic review, a qualitative review found that the fear of getting infected and spreading it to family members, high workload leading to frustration and exhaustion, physical problems related to the use of PPE, balancing work commitments with family life, as well as social discrimination and rejection were some of the major challenges identified in HCWs during the pandemic.6 A mixed-methods study done in Malawi among HCWs assessed how the pandemic-related experiences impacted their mental health. A wide range of mental health symptoms, profound emotional disturbances related to the rapid deterioration and death of patients, feeling overwhelmed due to their workload, and limited availability of resources were some of the themes identified. Fear of contracting the illness and infecting one's family members, disrupted social connections and family relationships, facing social stigma and discrimination, and being ostracized by their communities were observed to be major challenges faced by the HCWs.5 In various systematic reviews, concerns regarding acquiring the infection and transmitting it to their family members inadvertently, a lack of adequate PPE and other equipment, fear of quarantine, higher mortality associated with COVID-19, work burnout, and poor coping were reported.4,18 Similar findings, including work-related, family-related, and community-related issues, psychological problems, use of various coping strategies, etc., were observed in qualitative studies done in India among different categories of HCWs.12,19,20 In the present study also, all these themes were identified as the major ones that led to psychological problems among HCWs.
This study was conducted in a teaching hospital. Hence, we could capture the apprehensions of the residents during the pandemic. They expressed their anxiety of contracting and transmitting the infection, were overwhelmed by their work overload, and shared their experiences of hopelessness and learned helplessness related to patient care. Their main concern was regarding the lack of training in the subject that they had chosen to study. They were apprehensive about the deficiencies in their training during the pandemic, especially those in surgical specialties. These findings are discussed in detail elsewhere.21
As we face the threats of pandemics and epidemics in the future, we should ensure that the mental health of our HCWs is taken care of. For this, we need to build up the necessary infrastructure and materials, and ensure that adequately trained manpower is available in our hospitals. Screening the mental health of the HCWs and providing counselling and professional help may be required in such trying times. A caring attitude from higher authorities would help boost the morale of the HCWs.
Most quantitative and qualitative studies done during this period were conducted online. In this study, both the IDIs and FGDs were undertaken in person. The IDI interview schedules and FGD guides were developed separately and finalized after expert review. The FGDs were moderated by a person trained in qualitative research methodology. The data was analysed independently by four co-authors. Triangulation of methods, data, and researchers was ensured. This study aims to capture the apprehensions of residents at a teaching hospital during the pandemic. Although purposive sampling was employed to ensure the sample's representativeness, it may not have captured the total diversity of the study population. As the study was done among HCWs in a tertiary care teaching hospital, the findings may not be generalized to other healthcare settings.
CONCLUSION
In this qualitative study, psychological problems, including emotional and behavioral ones, as well as worries and apprehensions, were reported by all categories of HCWs during the pandemic. Interpersonal issues and interdepartmental problems added to their difficulties. Social stigma and related issues were observed among the nursing staff, nursing assistants, and attendants. Deficiencies in manpower, infrastructure, training, and materials were plaguing HCWs, while academic deficiencies were the major apprehension of the residents during the pandemic.
Conflicts of interest: Dr. Indu P.V. is an Emeritus editor of the journal. She was not involved in the peer review, decision-making, and processing of the article.
Other Authors: Nil
Source of funding: Nil
Ethical Approval: IEC - GMCKKD/RP2020/IEC/453 dated 06/07/2020
Author contribution section: IPV, HMT, AA, and VV contributed to the conceptualization and execution of the study. IPV and HMT conducted the In-depth Interviews. IPV moderated the Focus Group Discussions. CD, AZM, AP, AM, RKP, and HV assisted in the data collection and transcription. IPV did the translation. IPV, HMT, AA, and VV did data analysis and synthesis. IPV prepared the manuscript. All the co-authors reviewed the manuscript and approved the final version.
AI Declaration: The authors attest that there was no use of generative artificial intelligence (AI) technology in the generation of text, figures, or other informational content of this manuscript.
REFERENCES
- Ornell F, Halpern SC, Kessler FHP, de Magalhaes Narvaez JC. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cad Saúde Pública 2020; 36(4):e00063520. DOI: 10.1590/0102-311X00063520
- Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. General Psychiatry 2020; 33:e100259. [Link]
- Sun P, Wang M, Song T, Wu Y, Luo J, Chen L, et al. The psychological impact of COVID-19 pandemic on health care workers: a systematic review and meta-analysis. Front Psychol 2021; 12:626547. DOI: 10.3389/fpsyg.2021.626547
- Sheraton M, Deo N, Dutt T, Surani S, Hall-Favin D, Kashyap R. Psychological effects of the COVID 19 pandemic on healthcare workers globally: A systematic review. Psychiatry Research 2020; 292:113360. DOI: 10.1016/j.psychres.2020.113360
- Maliwichi L, Kondowe F, Mmanga C, Mchenga M, Kainja J, Nyamali S, et al. The mental health toll among healthcare workers during the COVID‑19 pandemic in Malawi. Scientific Reports 2024; 14:10327. [Link]
- Mathias EG, Anupama DS, Phagdol T, Nayal BS, Nagaraja B, Dickson K, et al. Impact of COVID-19 on mental health among healthcare workers in India: A mixed-methods systematic review. Oman Medical Journal 2023; 38(5): e544. DOI: 10.5001/omj.2023.111
- Narapaka PK, Katikala K, Ponnala VR, Meenakshi S, Viswas G, Singh M, et al. Psychological health among healthcare professionals during COVID‑19 pandemic: An updated meta‑analysis. Indian J Psychiatry 2024; 66: 413-20. DOI: 10.4103/indianjpsychiatry.indianjpsychiatry_173_23
- Grover S, Mehra A, Sahoo S, Avasthi A, Rao TS, Vaishnav M, et al. Evaluation of psychological impact of COVID‑19 on health‑care workers. Indian J Psychiatry 2021; 63:222-7. DOI: 10.4103/indianjpsychiatry.indianjpsychiatry_1129_20
- Visi V, Dutta G, Medhi GK, Bhattacharyya H, Sundaram SP, Pala S, et al. Psychological impact of Covid‑19 pandemic among the healthcare workers in a North‑Eastern state of India. J Family Med Prim Care 2022; 11:2756-62. DOI: 10.4103/jfmpc.jfmpc_1901_21
- George CE, Inbaraj LR, Rajukutty S, de Witte LP. Challenges, experience and coping of health professionals in delivering healthcare in an urban slum in India during the first 40 days of COVID-19 crisis: A mixed method study. BMJ Open 2020; 10: e042171. [Link]
- Razu SR, Yasmin T, Arif TB, Islam MS, Islam SMS, Gesesew HA, et al. Challenges faced by healthcare professionals during the COVID-19 pandemic: A qualitative inquiry from Bangladesh. Front Public Health 2021; 9:647315. DOI: 10.3389/fpubh.2021.647315
- Romate J, Rajkumar E. Exploring the experiences, psychological well-being and needs of frontline healthcare workers of government hospitals in India: a qualitative study. Humanities & Social Sciences Communication 2022; 9:89. [Link]
- Banerjee D, Rao TSS, Kallivayalil RA, Javed A. Psychosocial framework of resilience: Navigating needs and adversities during the pandemic, a qualitative exploration in the Indian frontline physicians. Front Psychol 2021; 12:622132. DOI: 10.3389/fpsyg.2021.622132
- Selvaraj P, Muthukanagaraj P, Saluja B, Jeyaraman M, Anudeep TC, Gulati A, et al. Psychological impact of COVID-19 pandemic on health-care professionals in India – A multicentric cross-sectional study. Indian J Med Sci 2020; 3:141-7. DOI: 10.25259/IJMS_193_2020
- Nayak BS, Surapaneni K, Sahu PK, Bhoi P, Dhananjay KVN, Silamban S, et al. The mental health of the health care professionals in India during the COVID-19 pandemic: a cross-sectional study. AIMS Medical Science 2022;9:283–92. DOI:10.3934/medsci.2022011
- Duden GS, Reiter J, Paswerg A, Weibelzahl S. Mental health of healthcare professionals during the ongoing COVID-19 pandemic: a comparative investigation from the first and second pandemic years. BMJ Open 2023; 13:e067244. [Link]
- Maunder RG, Heeney ND, Jeffs LP, Wiesenfeld LA, Junter JJ. A longitudinal study of hospital workers’ mental health from fall 2020 to the end of the COVID-19 pandemic in 2023. Scientific Reports 2024; 14:26137. DOI: 10.1038/s41598-024-77493-5
- Koontalay A, Suksatan W, Prabsangob K, Sadang JM. Healthcare workers’ burdens during the covid-19 pandemic: A qualitative systematic review. Journal of Multidisciplinary Healthcare 2021:14:3015–25. DOI: 10.2147/JMDH.S330041
- Chakma T, Thomas BE, Kohli S, Moral R, Menon GR, Periyasamy M, et al. Psychosocial impact of COVID-19 pandemic on healthcare workers in India & their perceptions on the way forward - A qualitative study. Indian J Med Res 2021; 153:637-48. DOI: 10.4103/ijmr.ijmr_2204_21
- Nair R, Mohan K, Jayakrishnan K, Srinivasan P, Javeth A, Sharma S, et al. Lived experience of nurses in COVID-19 units - A phenomenological study from Eastern India. J Caring Sci 2022; 11:197-209. DOI: 10.34172/jcs.2022.25
- Indu PV, Tharayil HM, Ayirolimeethal A, Vidyadharan V. Medical education during COVID-19: Perspectives from postgraduate residents. Indian J Psychol Med 2022; 44: 196–7. DOI: 10.1177/02537176211073781
|
Please cite the article as: Indu PV, Tharayil HM, Dilip C, Ayirolimeethal A, Harsha V, Padmanabhan A, Afeefa M, Rajula KP, Madathil AZ, Vidyadharan V. Psychosocial problems among healthcare workers in a tertiary care centre during the COVID-19 pandemic - A qualitative study. Kerala Journal of Psychiatry. 2025; 38(1): 11-23. |








