RESEARCH REPORT
|
|
Access the article online: https://kjponline.com/index.php/kjp/article/view/486 doi:10.30834/KJP.38.1.2025.486. Received on:29/10/2024 Accepted on: 07/05/2025 Web Published:28/05/2025 |
CLINICAL PROFILE OF PATIENTS ATTENDING THE MOTOR ACCIDENT CLAIM TRIBUNAL (MACT) BOARD IN A TERTIARY CARE CENTRE IN KERALA - A CROSS-SECTIONAL STUDY
Gopika Seena Sajith1, Deenu Chacko2*, Vidhukumar Karunakaran3
- Junior Resident, Department of Psychiatry, Government TD Medical College, Alappuzha
- Assistant Professor, Department of Psychiatry, Government Medical College, Ernakulam.
- Professor and Head, Department of Psychiatry, Government TD Medical College, Alappuzha
*Corresponding Author: Assistant Professor, Department of Psychiatry, Government Medical College, Ernakulam.
Email: deenusobin@gmail.com
INTRODUCTION
In India, 4,61,312 road accidents have been reported during the calendar year 2022, claiming 1,68,491 lives and causing injuries to 4,43,366 persons.1 Road traffic injuries account for nearly 10%-30% of hospital registrations, as highlighted by a study conducted in Bangalore.2
Recognizing the increasing burden of such accidents, the Motor Vehicles Act of 1988 established the Motor Accident Claim Tribunal (MACT), which became effective on 1st July 1989.3 This tribunal was designed to streamline the legal process by removing the jurisdiction of Civil Courts in motor accident cases, thereby expediting the resolution of claims. MACT is responsible for processing the claims arising from motor vehicle accidents and determining the compensation amount based on the evidence presented and the circumstances of the Road Traffic Accidents (RTA). The tribunal seeks the help of various medical boards in the state to assess the disability percentage following accidents.
The most common etiological factors for Traumatic Brain Injury (TBI) are falls, road traffic accidents, violent physical assaults, and injuries associated with athletic activities. Following a TBI, significant neurologic complications may occur, which include seizures, dementia, Alzheimer's disease, and cranial nerve injuries.4
The mental health consequences of TBI are personality changes, including impulsivity, severe irritability, affective instability, and apathy, usually within one-year post-injury.5 In the study of mental health consequences of Traumatic Brain Injury, attention has turned to cognitive, affective, and behavioral sequelae of injuries across the severity spectrum. These sequelae are often more disabling than residual physical effects. In addition, people may suffer from various psychiatric complications such as depression, post-traumatic stress disorder, generalized anxiety disorder, obsessive-compulsive disorder, and cognitive impairment that might significantly contribute to the comorbidity of the victims. Considering all the above complications, TBI is one of the significant public health burdens. Only about 25% of people achieve long-term functional independence following TBI.6 Understanding the clinical profile of these patients can facilitate their effective rehabilitation and provide them with the social and financial support they deserve.
There is a dearth of data regarding the clinical profile including the pattern of disability of patients attending the medical boards as instructed by the MACT. To the knowledge of the authors, this is the first study in the India in this population. This study aims to assess the clinical and disability profile of patients attending the MACT board of a tertiary care centre in Kerala.
MATERIALS AND METHODS
This is a record-based cross-sectional study of clinical profile, conducted on the patients referred to a tertiary care centre in Kerala for disability assessment by the MACT board. The study was initiated after clearance from the institutional ethics committee. The study period was one year, from January 1st ,2023, to December 31st, 2023
The inclusion criteria were the data of all patients who attended the MACT board during the study period. In MACT board assessment of disability is based on the disability guidelines of Government of India. The relevant data were entered in a predesigned proforma developed for the study The data collected included age, gender, district of MACT tribunal, time interval between RTA and disability assessment, percentage of disability, type of injury, type and site of brain injury, presence of disability (anyone with any percentage of disability is considered to have disability in the study), type of disability, type of psychiatric disability and the domains of IDEAS affected. Statistical analysis was done using R Statistical Software version 4.4.1 with its graphic user interphase 2.9-2., R commander (Rcmdr). The continuous data was expressed as mean with standard deviation, and categorical data was expressed as proportions with confidence intervals.
To assess the level of psychiatric disability among the patients attending the board, IDEAS (Indian Disability Evaluation and Assessment Scale) was utilised by the board members according to the manual for IDEAS. It is a standardized tool developed by the Rehabilitation Committee of the Indian Psychiatric Society to assess and quantify disability in individuals with mental disorders. It evaluates four key areas of functioning: self-care, interpersonal activities, communication and understanding, and work. Each domain is scored on a scale from 0 (no disability) to 4 (profound disability), along with the duration of illness with which the total score is added to obtain the global score The tool has a good internal consistency of (Cronbach’s alpha) of 0.892 and has good concurrent validity in disability estimation7.
RESULTS
The data of 248 patients were obtained by chart review.
Sociodemographic Data
The mean age of the patients was 44.2 years (S.D 14.9), and most were males (81.85%). The median time interval between the Road Traffic Accident (RTA) and the disability assessment in the MACT board was 5 years with an Inter Quartile Range (IQR) of 2 years. There were 8 (2.4%) patients who attended the board after 8 years of RTA. The patients who attended the MACT board belonged to different tribunals across southern Kerala. Most claimants were from Kottayam (27%) and Ernakulam (25.9%). (Table 1)
Table 1: Sociodemographic Profile
|
Sociodemographic Variables |
N (%) (N=248) |
|
|
Age (Years) |
<20 |
3(1.2%) |
|
20-40 |
102(41%) |
|
|
40-60 |
103(41%) |
|
|
>60 |
40(16%) |
|
|
Gender |
Male |
203(81.85) |
|
Female |
45(18.14) |
|
|
MACT Tribunal |
Number of Patients (%) (N=248) |
|
|
Alappuzha |
23(9.2%) |
|
|
Kollam |
43(17.3%) |
|
|
Ernakulam |
63(25.9%) |
|
|
Kottayam |
67(27%) |
|
|
Mavelikkara |
47(18.9%) |
|
|
Irinjalakkuda |
1(0.4%) |
|
|
Muvattupuzha |
1(0.4%) |
|
|
Paravoor |
1(0.4%) |
|
|
Pathanamthitta |
1(0.4%) |
|
|
Perumbavoor |
1(0.4%) |
|
Injury Profile
There were different types of injuries sustained by RTA, with the maximum number of patients having TBI, 90 (36.4%, 95% CI: 30.4-42.8), followed by upper and lower limb fractures. Among the patients who sustained TBI, the most common type of injury was subdural haemorrhage, and the cerebral lobe involved were the frontal, 54 (21.86%), temporal, 51 (20.65%), parietal, 43 (17.41%) and occipital, 4 (1.62%). (Table2)
Table 2: Injury profile
|
Types of Injuries |
|
|
TBI1 |
90(36.4%) |
|
Fracture upper limb |
68(27.42%) |
|
Fracture lower limb |
87(35.8%) |
|
Fracture spine |
27(10.8%) |
|
ENT/Ophthalmology |
22(8.8%) |
|
OMFS2 |
22(8.8%) |
|
Type of Lesion |
Number (%) |
|
Contusion |
29(32.2%) |
|
EDH3 |
24(26.6%) |
|
SAH4 |
32(35.5%) |
|
SDH5 |
45(50%) |
|
DAI6 |
5(5.5) |
|
Site of lesion |
|
|
Frontal |
54(21.86%) |
|
Temporal |
51(20.65%) |
|
Parietal |
43(17.41%) |
|
Occipital |
4(1.62%) |
1. Traumatic brain injury, 2. Oral and Maxillofacial Surgery,
3. Extradural Hemorrhage, 4. Subarachnoid Hemorrhage
5 Subdural Hemorrhage, 6 Diffuse Axonal Injury
Disability Analysis
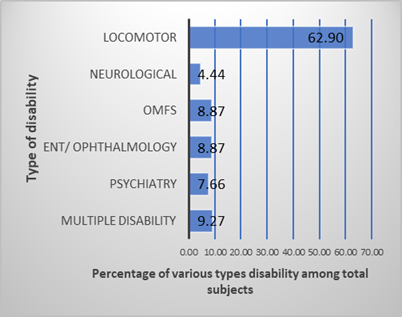
All the patients were assessed using IDEAS by the board members. Among the patients who attended the board, 196 (79.03%) had disability. The median disability percentage was 8, with an Interquartile range of 23.25 when the whole sample was studied. The most common disability sustained was locomotor type, 156 (80%). There were 11.7% of patients with multiple disabilities, i.e., those with more than one type of disability. (Table 3)
Table 3: Disability profile
|
Presence of disability |
Number (%) |
|
Yes |
196(79.03%) |
|
No |
52(20.96%) |
|
Types of psychiatric disability |
Number (%) |
|
Dementia due to head injury |
16(80%) |
|
Organic mood disorder |
1(5%) |
|
Secondary personality changes |
1(5%) |
|
Post-Traumatic Stress Disorder |
1(5%) |
|
Organic psychosis |
1(5%) |
|
Domain of IDEAS* impaired |
Number (%) |
|
Self-care |
8(42.1%) |
|
Interpersonal activities |
16(84.2%) |
|
Communication & understanding |
16(84.2%) |
|
Work |
18(94.7%) |
It was seen that among the patients with various disabilities, 9.74% (95% CI: 6-14.8) patients had psychiatric disability. For those with psychiatric disability, dementia due to head injury was the most common diagnosis (84%). The disability types of the whole sample are depicted in the bar chart. (Figure 1).
Figure 1. Bar chart showing the percentage of different types of disability
It was seen that 69.5% of those with psychiatric disability had some other type of disability as well. The mean IDEAS score of the patients with psychiatric disability was 8.6 (SD = 2.9). The work domain of IDEAS was the one found to be affected the most (94.7%), followed by communication and understanding, whereas the self-care domain was the least affected domain. The mean disability percentage was 23.8, and the median disability percentage was 45 among those with psychiatric disability.
DISCUSSION
Most studies on patients with RTA have revealed that accidents are common in young, productive age groups, leaving a tremendous financial burden on society. In 2019, road traffic injury was the leading cause of death for children and young people aged 5–29 years, and it was the 12th leading cause of death when all age groups are considered.8 If this trend continues by 2030, road traffic deaths will become the fifth leading cause of death. RTA is one of the leading causes of deaths, disabilities, and hospitalizations, with significant socioeconomic costs all over the world.9 Our study also shows that most patients coming to the MACT board following road traffic accidents are 20-40 years old.
Studies have shown that males are more involved in RTA. The deaths due to RTA continue to disproportionately impact men, with an overall female-to-male fatality ratio of 1 to 38,10. This can seriously affect the socioeconomic situation of the individual, family, society, and the nation. Our study also shows that most of those coming for disability evaluation in the MACT Board are males.
The motor accident claim tribunals are situated in various districts, and the tribunal usually refers claimants for disability evaluation to various medical boards constituted by the state; our centre also receives claimants from tribunals of other districts. The major share is from neighbouring districts like Kottayam and Ernakulam. As per data from report on road traffic accidents by Kerala government there is highest number of RTA as well as number of persons involved in Erankulam district compared to other districts in Kerala.11 The lack of proper disability assessment facilities in these districts, long waiting lists for assessments, and other administrative reasons may be speculated as the cause for the referrals from other districts. This can add to the difficulty of the claimants and the family as they need to travel long distances and spend a considerable amount of money due to the unavailability of boards in their native district. Another interesting finding the study revealed is that the median duration between RTA and disability evaluation is five years. This delay could also be due to the above-mentioned reasons, and it can adversely affect the patient and family regarding financial and social support.
The most common type of injury sustained was fracture of the upper and lower limbs, 63.22%, and the second most common injury was traumatic brain injury, which was 36.4%. Though abrasions, contusions, and lacerations are the most common types of injuries, our study was on patients referred for disability assessment, which usually involves grievous injuries. Subdural haemorrhage was the most common type of TBI in this study, which is in accordance with other studies. 12
Among those who came to the board, 79.03% had disability; this is an overestimate compared to the community prevalence of disability because the study was done in the context of disability evaluation. A study that assessed disability at 3 months following RTA had shown that the disability was seen in 16.36% of the patients.9
The study shows that among those who have a disability, 9.74 % had psychiatric disability. The relationship between TBI and psychiatric disorders is bidirectional. TBI can cause psychiatric disorders, including behavioural disorders and cognitive disorders; psychiatric disorders can increase the vulnerability to encountering an accident and sustaining TBI.4 Dementia with head injury was the most common psychiatric diagnosis, followed by secondary mood disorder, psychotic disorder, personality change, and post-traumatic stress disorder. High rates of mood, psychotic, and substance abuse disorders following TBI have been found in hospitalized trauma and tertiary care referral populations.13-16A study on psychiatric disorders and functional disability in outpatients with traumatic brain injury, it was found that 26% of the patients had current major depression, thus making them more functionally disabled and perceiving their injury and cognitive impairment to be more severe.14
In our study it was seen that locomotor disability was the most common type of disability, whereas multiple disability was seen in 9.3% of the patients, which includes more than one type of disability. A study done in the US has shown that approximately 50% of those with head injury have disability, and the disability is predominantly due to lower extremity mobility causing impairment in the work domain which is like our study.17
In a study of 20-year follow-up of patients with TBI, the importance of providing vocational rehabilitation services and support to overcome their disabilities, thus optimizing their community integration and work participation, was emphasized.18 Cognitive impairments persisting even after 3 months of TBI were found to be associated with higher percentages of disabilities.19 In moderate to severe TBI, cognitive recovery does not return to baseline even after 2 years of injury. The goal of cognitive rehabilitation following TBI is to enhance the person's ability to process and interpret information and improve the activities of daily living (ADL). Cognitive rehabilitation is most beneficial when administered as a part of a multidisciplinary or interdisciplinary approach rather than a “stand-alone” approach.20
This study was limited to data from the MACT board over one year, with no information on the rehabilitation status of patients with disabilities. Disability percentages may be underestimated as assessments were conducted 4-6 years post-injury. Additionally, the findings are not generalizable, as the study included only patients registered at a single tertiary care centre and sample size calculation not done. This was a record-based study, no assessment tool was administered by the investigators. Though the commonly reported psychiatric disorders are anxiety disorders and substance dependence after TBI we had none of them because the study was limited to those coming to MACT board having severe impairment. Future studies should aim for a broader and more representative sample with a prospective study design, incorporate real-time disability assessments, and evaluate long-term rehabilitation outcomes to provide a comprehensive understanding of the impact of RTA.
CONCLUSION
The study shows that the mean age of patients attending the MACT board was 44.2 years. And the majority were males. It was found that fractures were the most common type of injury sustained, followed by TBI; subdural haemorrhage was the most common type of TBI, and the frontal lobe was the most commonly involved lobe. The study shows that majority of patients who attended the disability board were disabled. TBI was the most common type of injury; among the patients with disability, the majority had locomotor disability. Among those with a disability, 9.74% had psychiatric disability. Dementia due to head injury was the most common psychiatric diagnosis. The median duration of head injury and disability evaluation was five years, and the majority of the patients came to the board from other districts and which emphasis the need for more assessment centres for disability preferably. This study brings forth the need for assessment of the pattern of disabilities in patients attending the MACT board and their clinical profile which is an unexplored area. Though we could not study the rehabilitation status of the patients, from the high prevalence of disability in the sample it is clear that there is lack of affordable rehabilitation services available for these patients. The study highlights the need for more awareness generation among the public regarding rehabilitation following TBI as well as more rehabilitation centers to bring down the disabilities. Alternative research of such kind could be conducted as a prospective study with a large sample and multicentric involvement, which could be beneficial in effective policymaking as well as aid in minimizing administrative delay in assessment procedure and rehabilitation thus alleviating the patient and care giver burden.
Funding: Nil
Conflict of interest: First and second author: nil
Third Author: Is the Emeritus Editor of the journal, but was not involved in the peer review, decision making, and copyediting of the manuscript.
"The author(s) attest that there was no use of generative artificial intelligence (AI) technology in the generation of text, figures, or other informational content of this manuscript."
REFERENCE
- Ministry of Road Transport and Highways releases Annual Report on ‘Road Accidents in India-2022 [Internet]. Press Release: Press Information Bureau. 2023 [cited 2024 Nov 4]. Available from: https://pib.gov.in/PressReleaseIframePage.aspx?PRID=1973295
- Gururaj G. Epidemiology of traumatic brain injuries: Indian scenario. Neurol Res. 2002;24(1):24–8. DOI: 10.1179/016164102101199503
- Ralte H, Vanlalhruaii, Lalmalsawma J, Lalnuntluanga K, Ralte H, Zohmangaihi P. The Evolution Of Motor Accident Claim Tribunal: A Study On Its Role In Justice Administration In India. Educ Adm Theory Pract. 2024 Jan 3;30(1):695–700. [Link]
- David AS, Fleminger S, Kopelman M, Lovestone S, & Mellers, J. Lishman’s Organic Psychiatry: A Textbook of Neuropsychiatry (Revised 4th Ed). (4th ed.) Wiley-Blackwell; 2009 .pp. 211. [Link]
- Howlett JR, Nelson LD, Stein MB. Mental Health Consequences of Traumatic Brain Injury. Biol Psychiatry. 2022 Mar 1;91(5):413–20. DOI: 10.1016/j.biopsych.2021.09.024
- Bicholkar A, Cacodcar JA. A study of road traffic injury victims at a tertiary care hospital in Goa, India. J Fam Med Prim Care. 2022 Sep;11(9):5490–4. DOI: 10.4103/jfmpc.jfmpc_693_21
- John S, Gupta PK, Sathe HK, Yadav P. Psychometric Properties of Indian Disability Evaluation and Assessment Scale in the Patients of Schizophrenia. Indian Journal of Social Psychiatry 39(4): 364-369. [Link]
- Global status report on road safety 2023 [Internet]. [cited 2024 Nov 4]. Available from: https://www.who.int/publications/i/item/9789240086517
- Dindi K, Bachani D, Singhal M, Singh AR. Road traffic injuries: Epidemiology, challenges, and initiatives in India. Natl Med J India. 2019 Mar 1;32(2):113. DOI: 10.4103/0970-258X.275355
- Chauhan A, Ahmed N, Singh JV, Singh VK, Singh A, Kumar S. Disability and mortality following road traffic injury: a follow-up study from a tertiary care center of India. Int J Community Med Public Heal. 2017 Nov 23;4(12):4712–7. DOI:10.18203/2394-6040.ijcmph20175356
- of Kerala, Department of Economics and Statistics. Road accidents in Kerala, 2018-2022. [Internet] [cited 2025 Mar 27]. Available from: https://www.ecostat.kerala.gov.in/storage/documents/79.pdf
- Chalya PL, Mabula JB, Dass RM, Mbelenge N, Ngayomela IH, Chandika AB, et al. Injury characteristics and outcome of road traffic crash victims at Bugando Medical Centre in Northwestern Tanzania. J Trauma Manag Outcomes. 2012 Feb 9;6(1):1. DOI: 10.1186/1752-2897-6-1
- Fedoroff JP, Starkstein SE, Forrester AW, Geisler FH, Jorge RE, Arndt SV, Robinson RG. Depression in patients with acute traumatic brain injury. Am J Psychiatry. 1992 Jul;149(7):918-23. DOI: 10.1176/ajp.149.7.918
- Fann JR, Katon WJ, Uomoto JM, Esselman PC. Psychiatric disorders and functional disability in outpatients with traumatic brain injuries. Am J Psychiatry. 1995;152(10):1493–9. DOI: 10.1176/ajp.152.10.1493
- Steffen-Allen FT, Marton KM, Graves L V., Ketchum JM, Silva MA, Loughlin JK, et al. Longitudinal Patterns of Alcohol Use Following Traumatic Brain Injury in an Active Duty and Young Veteran Military Sample: A VA TBI Model Systems Study. J Head Trauma Rehabil. 2022 Nov 1;37(6):350–60. DOI: 10.1097/HTR.0000000000000757
- Fujii D, Ahmed I. Characteristics of Psychotic Disorder Due to Traumatic Brain Injury: An analysis of case studies in the literature. J Neuropsychiatry Clin Neurosci. 2002;14(2):130–40. DOI: 10.1176/jnp.14.2.130
- Schneider ALC, Wang D, Gottesman RF, Selvin E. Prevalence of Disability Associated With Head Injury With Loss of Consciousness in Adults in the United States: A Population-Based Study. Neurology. 2021 Jul 13;97(2): E124–35. DOI: 10.1212/WNL.0000000000012148
- Andelic N, Howe EI, Hellstrøm T, Sanchez MF, Lu J, Løvstad M, et al. Disability and quality of life 20 years after traumatic brain injury. Brain Behav. 2018 Jul 1;8(7). DOI: 10.1002/brb3.1018
- Skandsen T, Finnanger TG, Andersson S, Lydersen S, Brunner JF, Vik A. Cognitive impairment 3 months after moderate and severe traumatic brain injury: a prospective follow-up study. Arch Phys Med Rehabil. 2010 Dec;91(12):1904–13.DOI: 10.1016/j.apmr.2010.08.021
- Barman A, Chatterjee A, Bhide R. Cognitive Impairment and Rehabilitation Strategies After Traumatic Brain Injury. Indian J Psychol Med. 2016 May 1;38(3): 172. DOI: 10.4103/0253-7176.183086
|
Please cite the article as: Gopika SS, Deenu C, Vidhukumar K. Clinical profile of patients attending the MACT board in a tertiary care centre in Kerala – A cross-sectional study. Kerala Journal of Psychiatry 2025; 38(1): 24-31. |








